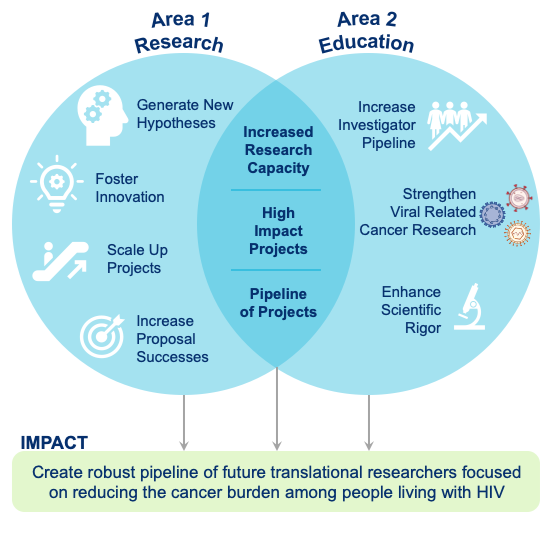
The Developmental Core (DC) aims to enhance capacity for cancer research through fostering the career development of junior investigators in South Africa, Zimbabwe, and the United States who have a demonstrated interest in infection-related cancer research among people living with HIV. This goal involves two broad strategies: 1) implementing a program that generates and supports rigorous pilot research projects and 2) providing other training and educational resources to enhance skills necessary for long term career success. The momentum created by this strategy would allow junior investigators at these sites to take advantage of pilot research funding opportunities and pursue career development. The supportive environment and highly experienced mentors will help ensure their long-term success as independent researchers. Moreover, this pipeline of highly trained researchers with interest in infection-related cancers among PLWH will meet the critical need for transdisciplinary, multi-institutional, and international partnerships to understand and potentially mitigate the rapidly growing cancer burden in Africa, where the prevalence of HIV infection remains high. The PAVILION DC program will help address this growing public health crisis by supporting junior investigators who can lead future research focused on cancers occurring among people living with HIV and ensure sustainability of research capacity, strength, and commitment.
The three DC Co-Leaders bring transdisciplinary expertise and mentoring experience across medicine, behavioral and population sciences, and cancer epidemiology.

Margaret Borok, MBChB, FRCP (University of Zimbabwe) is a Professor of Internal Medicine at the UZFMHS, with 20 years of experience in clinical research and research management, and manages the only referral clinic for patients with AIDS and Kaposi Sarcoma (KS). She is a member of the international committee and KS working group of the AIDS Malignancy Consortium (AMC) under the National Cancer Institute. Dr. Borok has a long history of mentoring clinician-scientists, especially those with a focus on AIDS-related malignancies.

Clement Gwede, PhD (Moffitt Cancer Center) is a Senior Member (Professor) in the Department of Health Outcomes & Behavior at Moffitt Cancer Center. is a community-minded, NIH-funded behavioral scientist who brings experience in mentoring students and junior investigators across multiple disciplines. At Moffitt, he has mentored 18 pre-doctoral trainees, nine post-doctoral fellows, and nine junior faculty as primary or associate mentor. In addition, Dr. Gwede participates as a grant writing and career development mentor in several national programs including the National Research Mentoring Network (NRMN)-Utah; Geographic Management of Cancer Health Disparities, Region 2; and the NCI’s 2022 Multi-level Training Institute (MLTI).

Taryn Young, MBChB, MMED, FCHPM, PhD (Stellenbosch University) is a Distinguished Professor, Head of the Division of Epidemiology and Biostatistics, and Director of the Centre for Evidence-based Health Care. She is a member of the Academy of Science of South Africa and the National Health Research Council, and is involved in the curriculum development, implementation and evaluation of training programs for under‐ and post-graduate students in public health and clinical epidemiology, biostatistics, evidence‐based healthcare and research synthesis. Professor Young is MPI of the Fogarty International Center funded D43 Africa Center for Biostatistical Excellence: Expanding biostatistical leadership for HIV/AIDS and TB Research..
Recurrent Respiratory Papillomatosis – A Forgotten Disease?
PI: Shaun Adam, Stellenbosch University
Recurrent respiratory papillomatosis (RRP) is a rare and serious disease caused by human papilloma virus (HPV). The condition is characterised by benign exophytic papillomatous growths in the larynx. There are more than 200 subtypes described and RRP is mainly caused by HPV subtypes 6 and 11. It is classically divided into juvenile-onset recurrent respiratory papillomatosis (JORRP, age < 18 years) and adult-onset recurrent respiratory papillomatosis (AORRP, age > 18 years). Notwithstanding the lower incidence and milder presentation of JORRP in developed countries, numerous studies have reported a dramatic decrease in the incidence following national vaccination programmes incorporating HPV subtypes that cause RRP. The reality is that the incidence of RRP remains high in the developing world, especially South Africa, and JORRP children often present with severe stridor requiring emergency surgery. Furthermore, the vaccination programme in South Africa does not include the HPV subtypes that cause RRP. This study is aimed at describing the incidence and prevalence of RRP seen at Tygerberg Hospital and the effect of vaccination on this group.
The molecular classification and HPV testing of histopathological specimens from HIV-infected and uninfected women with vulvar cancer at a tertiary hospital in a LMIC
PI: Jennifer Butt, Stellenbosch University
In LMIC, the main causative agent for vulvar cancer is HPV. HIV-infected women are at higher risk of persistent HPV infection and develop vulvar cancer at a much younger age. HPV-related vulvar cancer has a different pathogenesis, prognosis and recurrence rate to HPV-independent vulvar cancer, and yet the protocols for treatment are the same. It is of vital importance to classify vulvar cancers into these 2 molecular subgroups. This will allow investigation of HPV-related vulvar cancer as a separate entity and enable development of less morbid treatment protocols for these young women with vulvar cancer.
Collection of all available formalin fixed paraffin embedded tissue specimens from National Health Laboratory Services archives for women who had surgical treatment for vulvar cancer at Tygerberg Hospital between 2014 and 2021. Slides will be prepared for immunostaining and DNA extracted for HPV-testing. Immunohistochemical stains for p16 and p53 will be untaken with controls. PCR testing for high-risk HPV types will be performed.
Data will be entered in a Redcap database. Descriptive statistics comparing HIV-infected and uninfected patients with respect to p16 positivity, HPV types and number of HPV-types will be reported. Cox regression models will be tested for differences in mortality and recurrence.
This research should generate two articles in peer-reviewed journals.
Empowering Women, Enhancing Care: Knowledge, attitudes, and beliefs that impact health seeking-seeking behaviors among women living with HIV with vulvar precancer and cancer in Zimbabwe
PI: Tarisai Kufa, University of Zimbabwe
Women living with HIV (WLWH) face numerous health challenges, including an increased risk of developing vulvar precancer and cancer due to persistent human papillomavirus (HPV) infection. Contrary to studies suggesting that vulvar cancer primarily affects the elderly, WLWH experience this disease at a younger age. Additionally, vulvar-intra-epithelial neoplasia (VIN), a precursor to vulvar cancer, tends to be extensive, multifocal, and recurrent after treatment. Late-stage presentation is common among women with vulvar cancer, leading to poor outcomes with embarrassment, cancer-related anxiety, and lack of awareness about symptoms being highlighted as some of the reasons. This study aims to evaluate the factors impacting health-seeking behaviors in WLWH with vulvar precancer and cancer in Zimbabwe and describe their lived experiences. A mixed-method study will recruit WLWH with histologically confirmed VIN or vulvar cancer between January 2023 and April 2024. The study will be conducted at Newlands Clinic, an outpatient facility providing integrated HIV and sexual reproductive health services. Participants will be enrolled using convenience sampling and data will be collected using questionnaires and in-depth interviews. Thematic content analysis will be employed for qualitative analysis to identify recurring themes. Emerging themes will be noted in the margins, which will inform the development of a coding scheme. Descriptive statistics will be used for quantitative. Binary and categorical variables will be summarized using frequencies and proportions.
Determinants of late presentation of cSCC at a tertiary eye hospital in Harare, Zimbabwe
PI: Saiko Mangombe, University of Zimbabwe
Conjunctival squamous cell carcinomas (cSCC) originate in the squamous epithelium lining of the conjunctiva and commonly affect immunosuppressed individuals, particularly those living with HIV. While the timely diagnosis and treatment of these ocular cancers are crucial for optimal patient outcomes, a tertiary hospital in Zimbabwe, Sekuru Kaguvi Eye Unit (SKEU) reports an upward trend of late-stage cSCC presentation. At this stage of diagnosis, destructive eye surgery, orbital exenteration followed by radiation therapy are performed. We propose a pilot study that aims to explore the determinants of late-stage presentation of cSCC at SKEU. To achieve this, quantitative and qualitative data collection tools; open-ended and closed-ended questionnaires, and in-depth interviews will be used. Demographic, socio-behavioral and clinical factors, as well as knowledge, attitudes and practices of patients reporting with late-stage cSCC and will be compared to those of early-stage patients. To substantiate the qualitative findings from the patients, ophthalmologists and ophthalmic nurses at SKEU will be interviewed as key informants. The findings of this pilot study will inform early detection strategies, thus enhancing the overall clinical outcomes and prevention of morbidities that are associated with late-stage cSCC presentation.
Differences in expression levels of PIK3CA and TP53 in patients with cSCC stratified by HIV infection
PI: Nyarai Desiree Soko, University of Zimbabwe
Conjunctival squamous cell carcinoma (cSCC) is a rare ocular malignancy that disproportionately affects people living with HIV. Although its etiology is not fully understood, HIV infection and ultraviolet B radiation are established risk factors of cSCC. Thus HIV infection is postulated to disproportionately drive cSCC in populations living in Africa. The etipathogenic effects of HIV in driving cSCC carcinogenesis amongst people living with HIV is not known, however, development of squamous cell carcinomas is driven by alterations in the cell genome that lead to oncogene activation and tumour suppressor gene inactivation. Changes in these genes leads to dysregulation of normal cell growth and hence development of malignancies. Studying the transcriptome differences in biopsies from HIV infected individuals with cSCC and comparing them to those from HIV uninfected individuals with cSCC may help identify any differential gene expression related to HIV infection and hence drivers of carcinogenesis in HIV infected individuals. By examining tumours at the genomic and transcriptomic levels it is possible to better understand cancer biology and improve patient care, diagnosis and prognosis. We postulate that key cancer driving genes, oncogene PIK3CA and oncosuprressor TP53 are differentially expressed in patients with cSCC infected with HIV when compared to those with cSCC without HIV infection. Preliminary data from our research group on somatic variation differences in cervical cancer stratified by HIV status already shows differences in pathogenic mutation burden in HIV infected women with cervical intraepthilial neoplasia when compared to their HIV negative counterparts. It is therefore possible that HIV infection can result in somatic variation and resultant differential gene expression that can drive carcinogenesis. We propose therefore to investigate the differential expression of key cancer driving genes TP53 and PIK3CA in biospecimens obtained from patients with histopathologically confirmed cSCC who are infected with HIV when compared to patients with histopathologically confirmed cSCC who are not infected with HIV. We propose a 1:1 matched case control study, where cases are individuals with histopathologically confirmed cSCC who are infected with HIV and controls are patients with histopathologically confirmed cSCC who are not infected with HIV. Differential expression of TP53 and PIK3CA will be done on FFPE blocks using TaqMan gene expression assays. After mRNA expression levels for each group are quantified using the 2(-DeltaDelta C(T)) method; two-tailed unpaired t-test or Mann-Whitney U will be employed to assess differences in expression levels of PIK3CA and TP53 stratified by HIV status.